Cavitational lesions may produce no symptoms at all, especially if we find no redness over the area or signs of drainage. However, these lesions may also produce intense, trigeminal neuralgia-like symptoms, which cause suffering to such an extent that it’s a wonder patients can stand the pain and suffering.
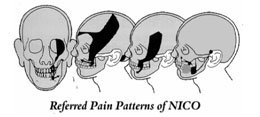
There are established, characteristic referred pain patterns (Figure 1), which we find very consistent in most symptomatic cavitation cases. Patients with pain usually have an underlying, constant dull aching. Along with this gnawing, deep pain, often there’s a sharp, shooting pain, which, understandably, convinces doctors that the diagnosis is trigeminal neuralgia.
A very common symptom we find is a sour, persistent drainage from the cavitation directly into the mouth. This foul taste makes many patients and doctors alike consider a diagnosis of sinusitis. Unfortunately, all the sinus surgery in the world will not correct the problem if the sour fluid is draining from areas of dead bone, namely, a jawbone cavitation
To confuse matters more, many patients report systemic symptoms like arm or leg pain and generalized fatigue. We’ve seen these systemic symptoms improve, or completely resolve, once the cavitation (or cavitations) is removed. The same has been seen in some chronic fatigue cases.
The most common scenario we see usually starts with a simple dental restoration. The family dentist replaces an old restoration (filling) and the tooth becomes sensitive, especially to cold temperatures. The doctor may replace the filling again or several more times, but the sensitivity never decreases. Then, in most cases, the tooth is treated with root canal therapy. But guess what? The pain continues. Another doctor is consulted, only to have the tooth re-treated with root canal therapy, but the pain persists . . . generally worse than in the beginning. Finally, out of sheer desperation (of both patient and doctor), the tooth is extracted, only to have the pain continue and intensify.
In this scenario, the finest dentistry was performed, but something went wrong. It wasn’t neglect by the dentist but damage to the tiny vessels in the jaw around and beneath the injured tooth. Due to the constant inflammation and swelling, an infarction occurs in one or more of the tiny vessels, producing ischemia and, ultimately, bone death and cavitation formation (Figure 2).
Remember, cavitations may be completely painless. This is not unique to the jawbones. In other bones, such as the femur, often there is no pain even when the bone destruction is extreme.
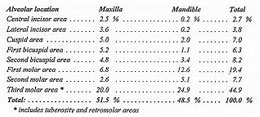
In the last several years, the term cavitation has been used to describe various bone lesions which appear both as empty holes in the jawbones and holes filled with dead bone and bone marrow. In Table 1, common locations of NICO lesions are listed. Note that the most common locations overall are areas of wisdom teeth (third molars).
Often, these NICO lesions take years to develop, usually producing few if any symptoms . . . for a while. Then, generally for unknown reasons, pain in the jaws, face, head and neck may develop. There are characteristic referred pain patterns, which generally confuse patients and doctors alike (Figure 2).
The results of recent research of Dr. Boyd Haley (former Chairman, Department of Chemistry, University of Kentucky) show that ALL cavitation tissue samples he’s tested contain toxins, which significantly inhibit one or more of the five basic body enzyme systems necessary in the production of energy. These toxins, which are most likely metabolic waste products of anaerobic bacteria (bacteria which don’t live in oxygen), may produce significant systemic effects, as well as play an important role in localized disease processes, which negatively affect the blood supply in the jawbone. There are indications that when these toxins combine with certain chemicals or heavy metals (for example, mercury), much more potent toxins may form.